Thermal disinfection of laundry in the care industry: definition, guidelines and procedures for handling soiled laundry in healthcare environment
Over the course of this guide we’ll be walking you through the true definition of thermal disinfection with regards to laundry in the care sector, as well as the guidelines and procedures that you need to be paying attention to, and the most effective laundry equipment to counter the risk of infection.
Laundry in the care sector: an overview
Laundry practice in the healthcare sector can either act as the gateway to infection outbreak, or the key to infection prevention.
While it might not be for the faint hearted, the fact of the matter is that linen and other textiles, such as sheets, towels and patients/residents personal clothing, is likely to come into contact with any manner of bodily fluids; some of which could contain very harmful microbes such as bloodborne pathogens or Clostridium difficile (C-diff).
HTM01-04, the health service guideline which specifies the hospital laundry arrangements for used and infected linen, splits it into three categories:
- Used (soiled and fouled) linen: This covers all used linen from non-infectious patients.
- IInfected linen: Any laundry that has come into contact with patients suffering from any one of a predetermined list of infectious conditions
- Heat Labile: Linen that could become damaged by exposure to wash temperatures above 40˚C
What is the true definition of thermal disinfection?
Interestingly, our definition of contaminated laundry in Australia is different many other parts of the world, where they have separate processes depending on whether linen is fouled or infected. Here, regardless of whether a resident has wet the bed, or contracted a healthcare associated infection (HCAI), the linen should be considered ‘red bag’ washing.
When it comes to handling soiled laundry, thermal disinfection – coupled with a proper laundry cycle management system – is the overarching way to stop the spread of infection in its tracks. But, is it just a ‘hot wash’?
In short, thermal disinfection is the use of above-average wash temperatures for a set cycle time to ensure any potentially infections microbes are killed. This can be done in a number of ways, such as 93°C for one minute, 71°C for three minutes, or 65°C for at least ten minutes Crucially, these temperatures are suitable for use when washing both ‘used’ and ‘infected’ linen.
However, wash cycles which are neither hot enough nor long enough will not be able to fully destroy the potentially infectious pathogens.
Although using the above temperatures will kill any bacteria within the wash cycle, this should not be viewed in isolation as an effective means to prevent infection outbreaks, as failing to adequately separate soiled and clean laundry could easily lead to reinfection. More on that later.
What are key guidelines operators should refer to?
Given the sensitive nature of the care sector, there are a number of official industry guidelines in place to provide laundry operators with the necessary clarity as to how to run their laundry in a safe and effective way.
An integral, but not exhaustive, list of best-practice guidelines can be found below:
COSHH regulation (Control of Substances Hazardous to Health)
The COSHH regulation place requires the operators to identify substances that have the potential to cause harm or ill health and to ensure that any such risks are removed, reduced and controlled.
The Hospital Laundry Arrangements for Used and Infected Linen provides an overview of the recommended procedures to help healthcare operators correctly handle and launder linen. As well as covering the importance of securing the disinfection of used and infected linen, this comprises of the basic principles of infection control.
The Choice Framework for local Policy and Procedures for Decontamination of linen for health and social care sectors is a four-part document that offers guidance on the most effective ways to clean linen in healthcare environments, including the testing and validation of laundry washing equipment.
BS EN 14065 is the internationally recognised standard for certifying biocontamination control systems for the laundry processing of textiles.
Australian standard for laundry practice.
What procedures can be put in place to prevent infection?
Beyond ensuring thermal disinfection has taken place, there are a few absolutely key processes laundry operators in the healthcare industry can employ to guarantee thermal disinfection.
Outsourcing laundry vs on-premises laundry
While some healthcare sites continue to outsource their laundry, doing so risks linen being exposed to a number of different contaminants, above and beyond those linked to the healthcare sector. Crucially, operators do not have full control of the transportation process, so in all honesty can have no guarantee that outsourced laundry is cleaned to the required standards. As such, all hospital and healthcare environments should employ an on-premises laundry, to ensure that all linen is washed in line with infection control laundry guidelines.
Avoiding recontamination of freshly washed laundry is also essential for preventing infection. After all, there is little point achieving full thermal disinfection of soiled linen, only for it to become contaminated again; especially as human contact is one of the fastest ways for bacteria to travel. In fact, it is advised that items are handled no more than four times once washed.
With that in mind, operators should be prepared to implement a dedicated laundry cycle management process which covers the entirety of the operation, from contamination and collection, through to washing and storage.
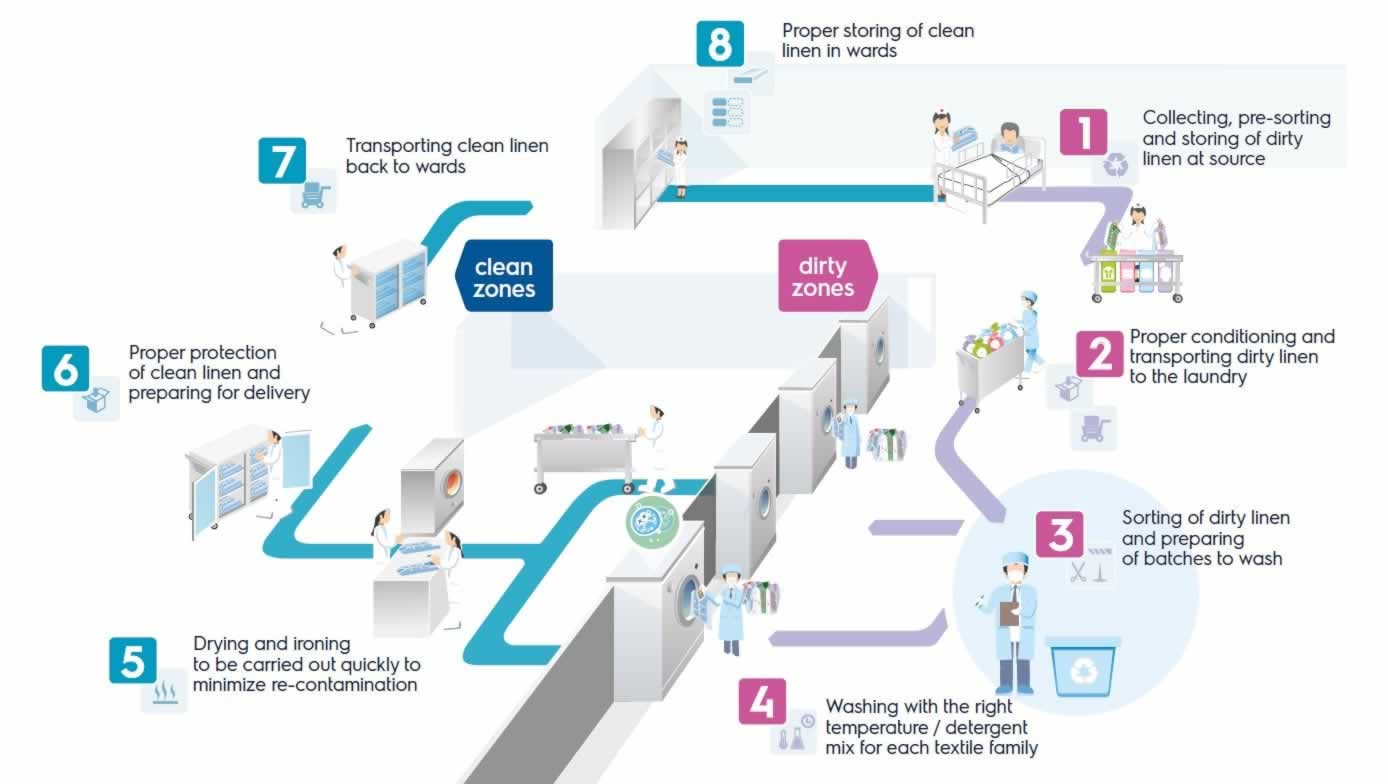
The eight-step process is based around the Risk Analysis Biocontamination Control (RABC) principle, which helps to identify the dangers within any given environment, and establish the correct target levels and tolerances for each potential hazard.
With that in mind, a laundry cycle management system gives operators detailed help with each stage of the journey, explaining how linen should be collected, transported, washed, dried, packed, transported and ultimately stored once clean.
What’s the best equipment for preventing laundry contamination?
Having outlined the importance of taking a holistic view of laundry cycle management, we can now delve down into the physical process of the wash cycle, and which equipment can help guarantee full thermal disinfection.
One of the safest ways to achieve this is to employ a barrier washing system, which ensures that items are loaded from one side of the machine when dirty and unloaded from a separate, clean side when the wash cycle is complete. This eliminates the need for operators to re-enter an unhygienic environment and, consequently, minimises the risk of linen being re-contaminated once it has been cleaned.
Operators can also gain further piece of mind by employing tools that can validate the wash temperatures of each cycle.
To sum up…
Ultimately, laundry practice for hospitals, healthcare sites, or aged care facilities can be make or break when it comes to preventing infection. Given the high volume of potential contaminants likely to find their way into healthcare linen, failing to achieve full thermal disinfection could easily pave the way for future outbreaks.